E-LOG GENERAL MEDICINE
★ CASE SCENARIO
A 40 year old male patient who is RTC driver by profession came to the OPD with chief complaints of :
- fever since 3 days
- Headache since 2 days
★ HISTORY OF PRESENT ILLNESS :
- Patient was apparently asymptomatic 3 days back , the he developed fever which is of high grade and associated with chills , not associated with any diurnal variation
- There is H/O headache since 2 days in frontal region which is of continuous in nature
- No H/O nausea , vomiting , loose stools , blurring of vision , abdominal distension , cough , cold
★ HISTORY OF PAST ILLNESS
- No H/O DM , HTN , Bronchial asthma , TB , epilepsy
★ TREATMENT HISTORY
- There is no usage of drugs as of now.
★ PERSONAL HISTORY
- Married
- Mixed diet
- Appetite - Normal
- Bowel movements - regular
- Micturation - normal
- No known allergies
- Ocassional alcoholic since 2 years [ last alcohol consumption 10 days back ]
★ FAMILY HISTORY
- Not significant
★ GENERAL EXAMINATION
- No - pallor / cyanosis / lymphadenopathy / malnutrition / icterus / clubbing / oedema / dehydration.
- Temperature : 99°F
- PR : 84/min
- RR : 16/min
- BP : 110/70 mmHg
- Spo2 : 98% at room air
- GRBS : 134mg/dl
★ SYSTEMIC EXAMINATION
— CVS
- Thrills : No
- Cardiac sounds - S1 , S2 heard
- Cardiac murmurs : No
— RS
- Dyspnea : No
- Wheeze : No
- Position of Trachea : central
— ABDOMEN
- Shape of abdomen : Obese
- No tenderness , palpable mass
- Hernial orrifices : Normal
- No fluids , bruits
- Liver and Spleen are not palpable
- Bowel sounds : no
— CNS
- patient is conscious
- speech is normal
- No signs of meningeal irritation
- No focal neurological defect is seen
— Reflexes
- plantars - flexor
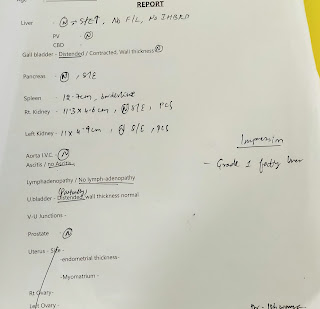
INVESTIGATIONS
2/3/2022






Comments
Post a Comment